Transcatheter Aortic Valve Implantation (TAVI)
Referral for Transcatheter Aortic Valve Implant
You have been diagnosed with a condition called aortic stenosis, a narrowing of the aortic valve. Your doctors have recommended a valve replacement using Transcatheter Aortic Valve Implant (TAVI) to treat your aortic stenosis. This site gives you information about TAVI to help you and your family prepare for your hospital stay. This information is a general guide and as everyone is different please seek personal advice from a qualified healthcare professional. Be sure to ask us if you have any questions and we will be happy to answer your questions and assist you.
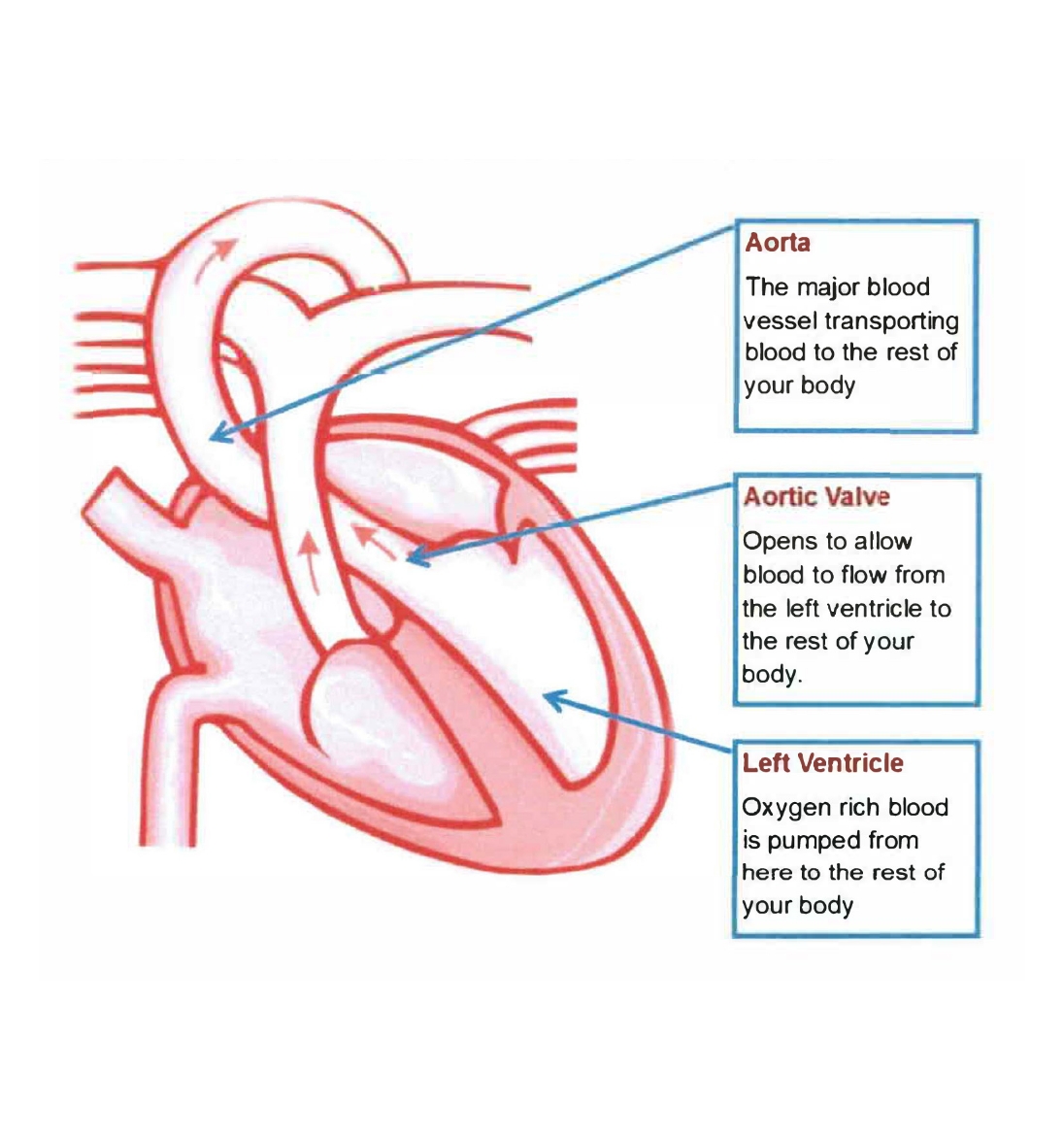
Your Heart and Valves
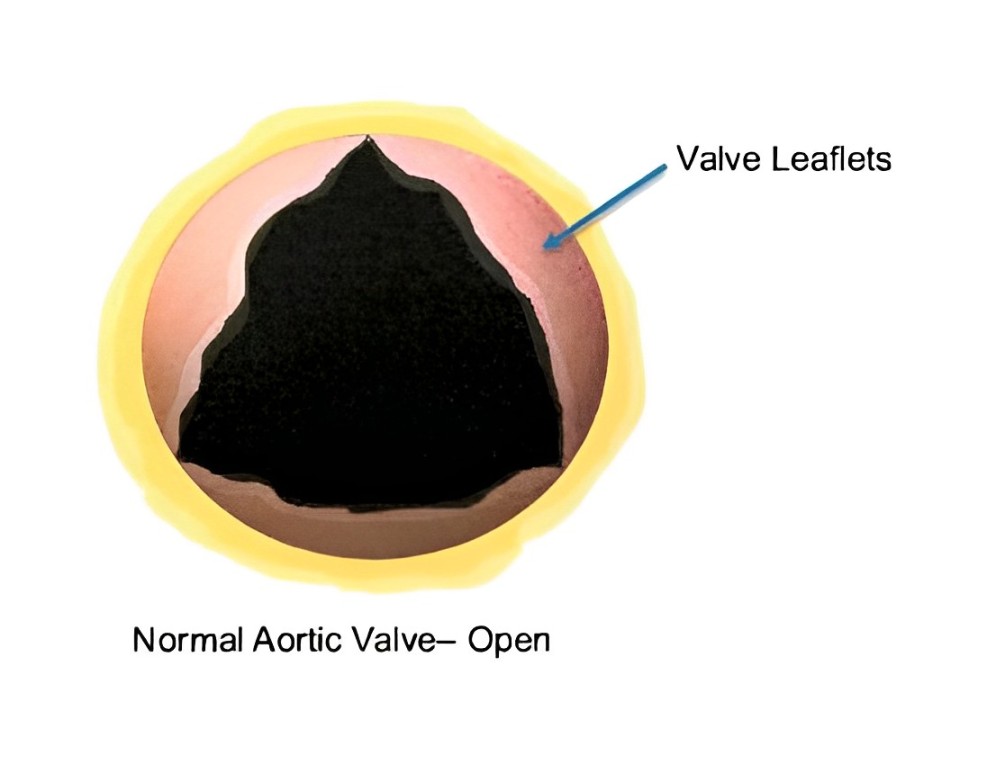
Your heart is a muscle that pumps blood around the rest of your body. There are four chambers of the heart, each with a valve with two or three leaflets. Your valves act as doors that open and close to allow blood to flow in one direction through the heart.
What is Aortic Stenosis?
Your aortic valve is on the left side of your heart and opens to allow blood to flow out of your heart, from your left ventricle, to your aorta which is a major blood vessel that circulates oxygen rich blood to the rest of your body. The leaflet then closes to stop the blood from flowing back into the left ventricle of your heart.
Aortic stenosis occurs when there is a build of calcium deposits on the valves leaflets. The valve then becomes narrowed and cannot open or close properly. This means that the blood within the heart is not able to flow easily through the valve and the heart has to work harder to pump the blood to the rest of your body. Blood may also flow backwards into the heart, known as aortic regurgitation. As a result less oxygen rich blood is pumped to your brain and rest of your body which can cause symptoms.

What are the symptoms of Aortic Stenosis?
Shortness of breath
Tiredness
Feeling dizzy or fainting
Palpitations or feeling that your heart is racing
Swollen ankles or legs
Chest pain
Treatment Options
The traditional treatment for people with severe aortic valve problems involves open heart surgery to repair or replace the aortic valve. Some people cannot have heart surgery due to their age or medical condition as it would be too risky. These people may be suitable for a less invasive procedure called a Transcatheter Aortic Valve Implantation (TAVI). Only a specialised Heart Team can decide if this treatment is for you.


Who is the Heart Team Involved in Your Care
TAVI Cardiologist
TAVI Nurse Coordinator
Geriatrician Intensive Care
Specialists Vascular Surgeon
What are the alternatives?
If you and your Heart Team decide that TAVI or surgical aortic valve replacement is not for you the following alternatives may be available for you after consultation with your Cardiologist;
Medication therapy may control your symptoms, but will not be able to treat your aortic valve disease.
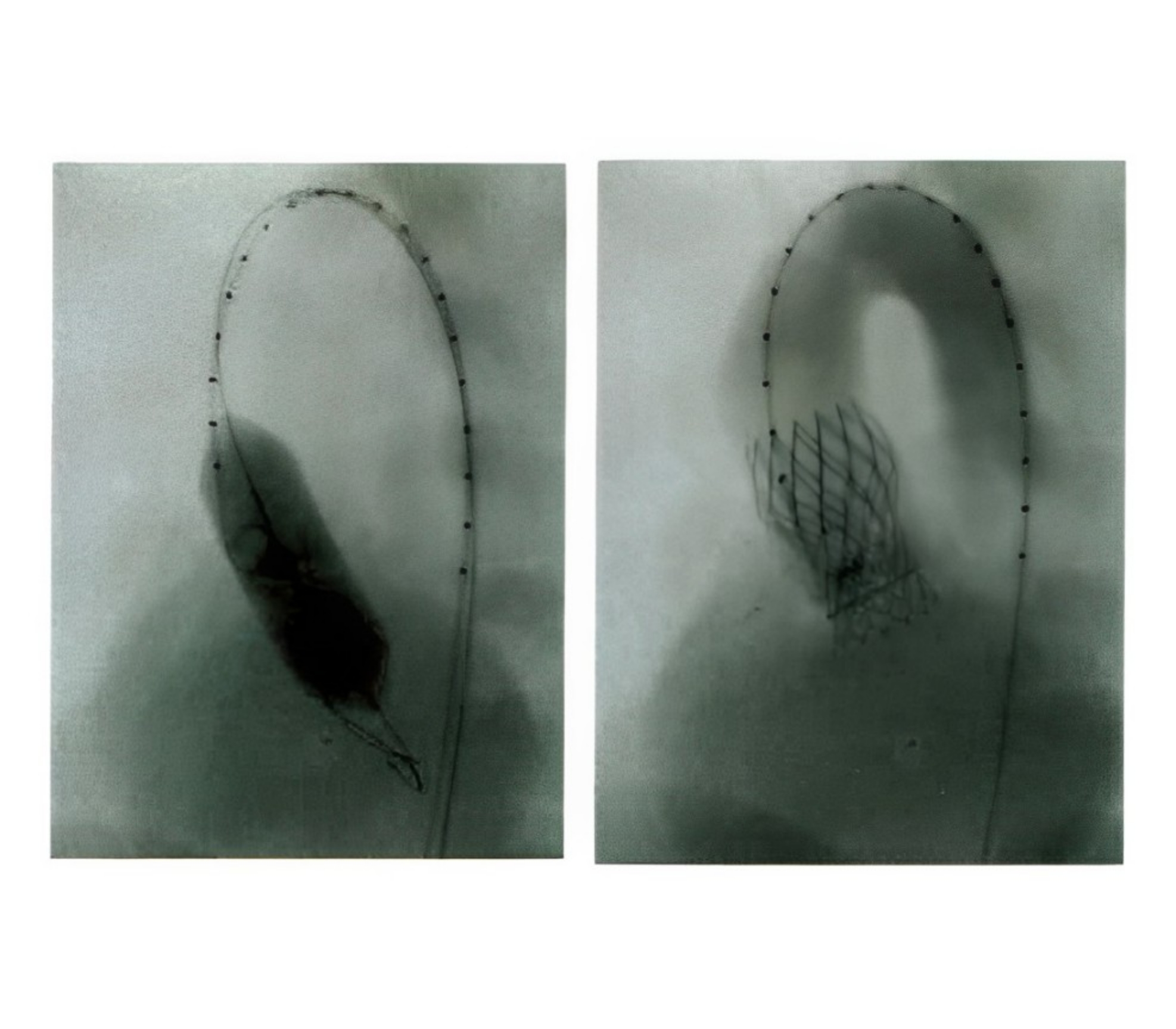
Balloon Valvuloplasty, where a catheter with a balloon on the tip is guided using x-rays and ultrasound to the diseased aortic valve. The balloon is then inflated to open the valve. Ballooning of the valve is often not a long term solution as the valve can become narrowed again, but can provide some short term symptom relief.

After you have been referred to the TAVI Heart Team, we need to complete some tests to find out if TAVI is right for you
These tests include:
Small sticky dots (electrodes) are put on your skin on your chest, arms and legs to record your heartbeat. It is a painless and takes 10 minutes.
A physical examination- medical examination of your body performed by a health specialist.
A sample of blood is taken from a vein in your arm to look at different areas of your general health. What we are checking can be explained by the nurse taking the test.
Sound waves are used look at the structure (chambers and valves) of your heart by getting a moving picture (ultrasound image)
A special x-ray test that gives us a 3-D picture of your body. The picture is more detailed than an x-ray, can take up to an hour and you will be given a special dye so we can see blood vessels clearly Coronary angiogram (cardiac catheterisation) – A special x-ray to look at the main blood vessels that supply your heart. During the procedure a catheter is guided through a small incision in your groin or wrist to your heart. A special dye (contrast) is then injected through the catheter so they appear on the x-ray. The procedure is done under local anaesthetic and usually takes about 30-45 minutes
we will ask you to walk for 6 minutes and see how far you can walk
we will ask you to blow into a tube so we can see how well your lungs work. This is painless and usually takes about 10
Other Tests May Be Required Include:
looking at the blood vessels of the heart
more detailed look at the heart done by swallowing a ultrasound probe under sedation
looking at the blood vessels of the neck
Along with the above tests you will need to see a Geriatrician and a Cardiothoracic surgeon for an assessment on your overall health and suitability for a TAVI procedure.

What To Bring With You During The Tests
A list of your medications
A support person such as a partner, child or good friend who knows you well and can help provide the team with information about you.
What Happens During The Heart Team Meeting
Once you have completed all of your workup tests, the TAVI Nurse Coordinator and a doctor will put all of your results together to present to the heart team.
This information is presented confidentially and a discussion had between the members to decide on if you are suitable for TAVI or require other management.
Once a decision has been made you will be notified by the TAVI Cardiologist
What are the risks?
Your doctor has recommended you for a Transcatheter Aortic Valve Implantation (TAVI) as they believe the overall benefits to you outweigh the risk of not going ahead with the procedure. There are risks and complications related to this procedure. They include but are not limited to the following.
Minor swelling or bruising at the puncture site.
Aneurysm or pseudoaneurysm of the femoral artery which may need to be surgically repaired or stented (a tube placed inside the vessel to stop the leak).
Hypertension/hypotension (high or low blood pressure).
Abnormal heart rhythms that may require permanent pacemaker implantation.
Bleeding from the groin which you may need a blood transfusion for.
Increased risk of wound infection, chest infection, heart and lung complications.
Blood clots in the lungs (Pulmonary embolism) or leg (DVT) causing pain and swelling.
Infection needing antibiotics.
Stroke (blood clot or bleeding in the brain) this may cause long term disability.
Heart attack caused by the new valve blocking your coronary arteries (which supply your heart muscle with blood and oxygen).
A punctured lung that needs a tube to be put in to your chest to reinflate the lung.
Worsening or failure of kidney function that may need dialysis.
Skin injury from radiation. This may cause reddening of the skin
Accidental tear or puncture of the blood vessels, myocardium (heart muscle), aorta (major artery) or valve structures which may need emergency major surgery.
The valve moves from its position, this may need to be removed with a special catheter or open heart surgery.
Infection of the new valve.
Large leakage around new valve.
Death as a result of this procedure is rare.
Before Your Procedure
The Coordinator will call you to inform you of the procedure booking.
You will need to attend the Pre Admission Clinic 1-2 weeks before your procedure. The Coordinator will let you know the date of this appointment. At this appointment you will have an education session with the Coordinator, see an Anaesthetist (sleeping doctor), see the TAVI Cardiologist for consent, as well as have some blood tests and a chest x-ray. Please bring your medications and a support person with you for this appointment.
Please see your dentist 2 weeks before your procedure and get a letter to clear you of any active infection. If there is an infection you may need to have this fixed before your TAVI procedure. Please inform the Coordinator of any issues.
The night before and morning of your procedure you will need to have a shower with a special surgical wash. You will get this at the Pre Admission Clinic.
Do not eat anything 6 hours before your procedure (from midnight), you may drink only clear fluids up until 2 hours before your procedure.
Please let us know if you are allergic to Iodine, Contrast or any other medications.
Ask any questions that you or your family may have and sign a form consenting to the procedure.
Please arrange a friend or family member to take you home from hospital and stay with you for your first 2 weeks at home. You cannot go home alone or in a taxi.
You will change into a hospital gown, be given an ID armband. You will have all hair clipped from your knees to your neck on admission to hospital. Your healthcare team will take your vital signs (blood pressure and pulse) and insert an IV (intravenous) line into a vein in your arm.
How long does a TAVI Procedure take?
The procedure will take approximately 2 hours.
Medication Information
Below is a list of medications with instructions on when to stop them.
| MEDICATION NAME | OTHER NAMES | WHEN TO STOP |
|---|---|---|
| ACE Inhibitors | Captopril, Ramipril, Perindopril, Avapro, Irbesartan, Micardis, Atacand | 2 days before |
| Alternative Medicine | Herbal, Green tea, Fish Oil, Glucosamine, Garlic Tablets | 7 days before |
| Anti-Inflammatory Drugs | Actiprofen, Brufen, Celebrex, Dolobid, Feldene, Indocid, Naprogesic, Naprosyn, Voltaren | 7 days before |
| Aspirin | Astrix, Cartia, Cardiprin, Dispirin, Solprin | DO NOT STOP |
| Beta-Blockers | Acebutolol, Atenolol, Betaxolol Bisoprolol, Carvedilol, Esmolol, Labetalol, Metoprolol, Nadolol, Nebivolol, Sotalol, Propranolol, | 2 days before |
| Dipyridamole | Persantin, Asasantin | 7 days before |
| Metformin | Diabex, Diaformin, Formet, Gluhexal, Glucomet, Pioglitazone, Janumet | 2 days before |
| NOACs | Rivaroxaban, Xarelto, Apixaban, Eliquis, Dabigatran, Pradaxa | 3 days before |
| Prasugrel | Effient | 7 days before |
| Empagliflozin or Dapagliflozin | Jardiance, Jardiamet, Xigduo XR,Forxiga, Glyxambi, Qtern | 3 days before |
| Ticagrelor | Brillinta | 7 days before |
| Warfarin | Coumadin, Marevan | 5 days before |
The TAVI Nurse Coordinator will confirm all your medications at the Pre Admission Clinic visit.
How long will you stay in hospital
Most people stay in hospital for 1 to 4 days
During the TAVI
For the TAVI procedure you do not always need a general anaesthetic, this will be discussed with you during your pre admission clinic appointment. You will be sleepy and relaxed and if needed a breathing tube will be placed down your windpipe, this will be removed at the end of the procedure or when you are ready to breathe on your own. If you do not need a general anaesthetic you will be made sleepy and relaxed but able to breathe on your own, with an Anaesthetist monitoring you during the whole procedure.
A drip will be put into a vein in your neck or arm to give you fluids and medications. A drip will be put into an artery in your arm to monitor your blood pressure.
A urinary catheter will be put into your bladder, you may feel like you need to pass urine, but the catheter will drain the urine away by itself.
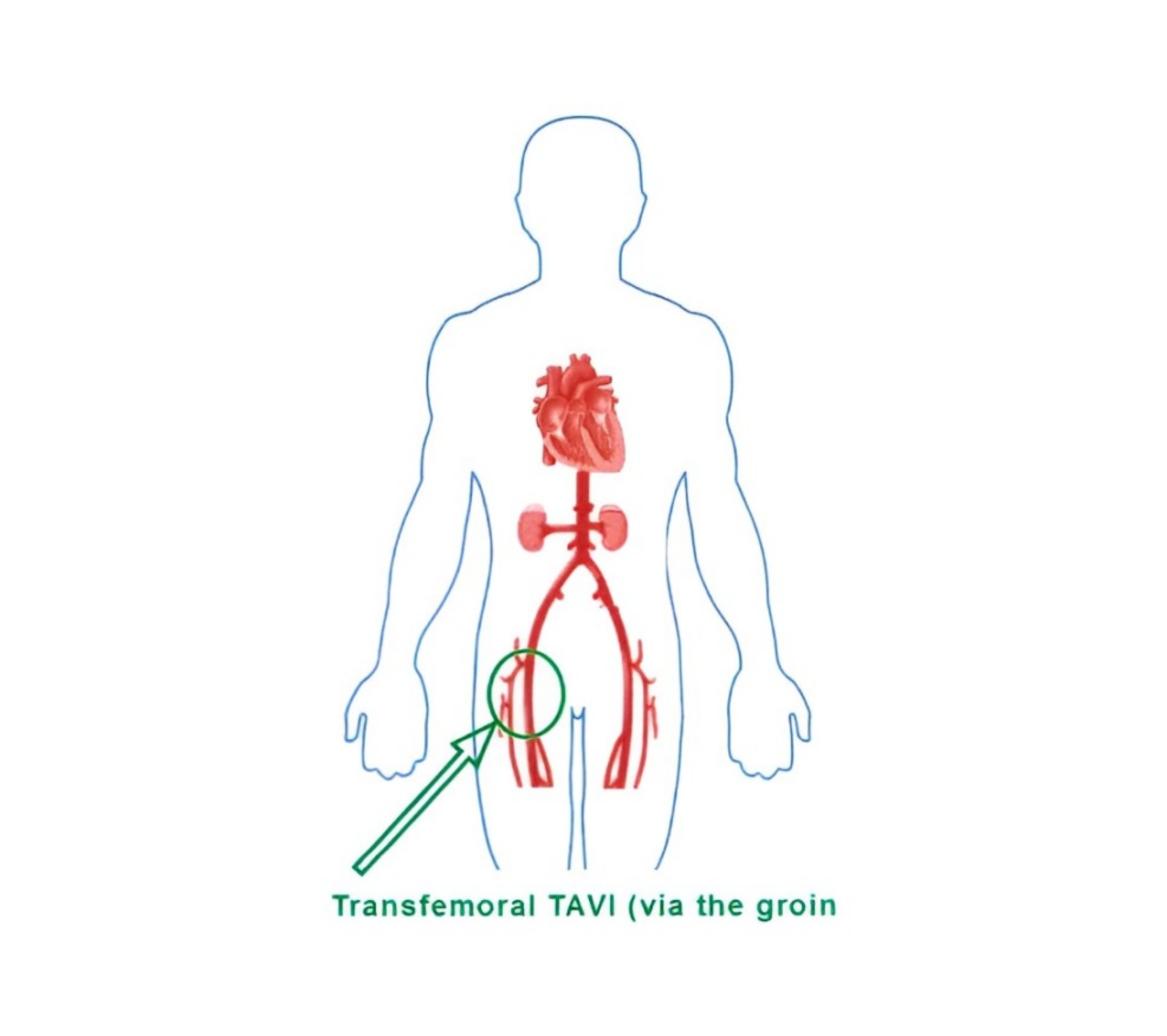
The aortic valve is implanted through a small cut in your groin (transfemoral). A catheter (thin flexible tube) is inserted through the cut and floated up to your heart and valve.
Contrast dye (iodine) is injected to look at the blood vessels that go to your heart.
A temporary pacemaker wire will be placed in the right side of your heart via the blood vessels in your groin to speed up your heart during the valve insertion for approximately 30 seconds. This is to help with putting the valve in the correct place.
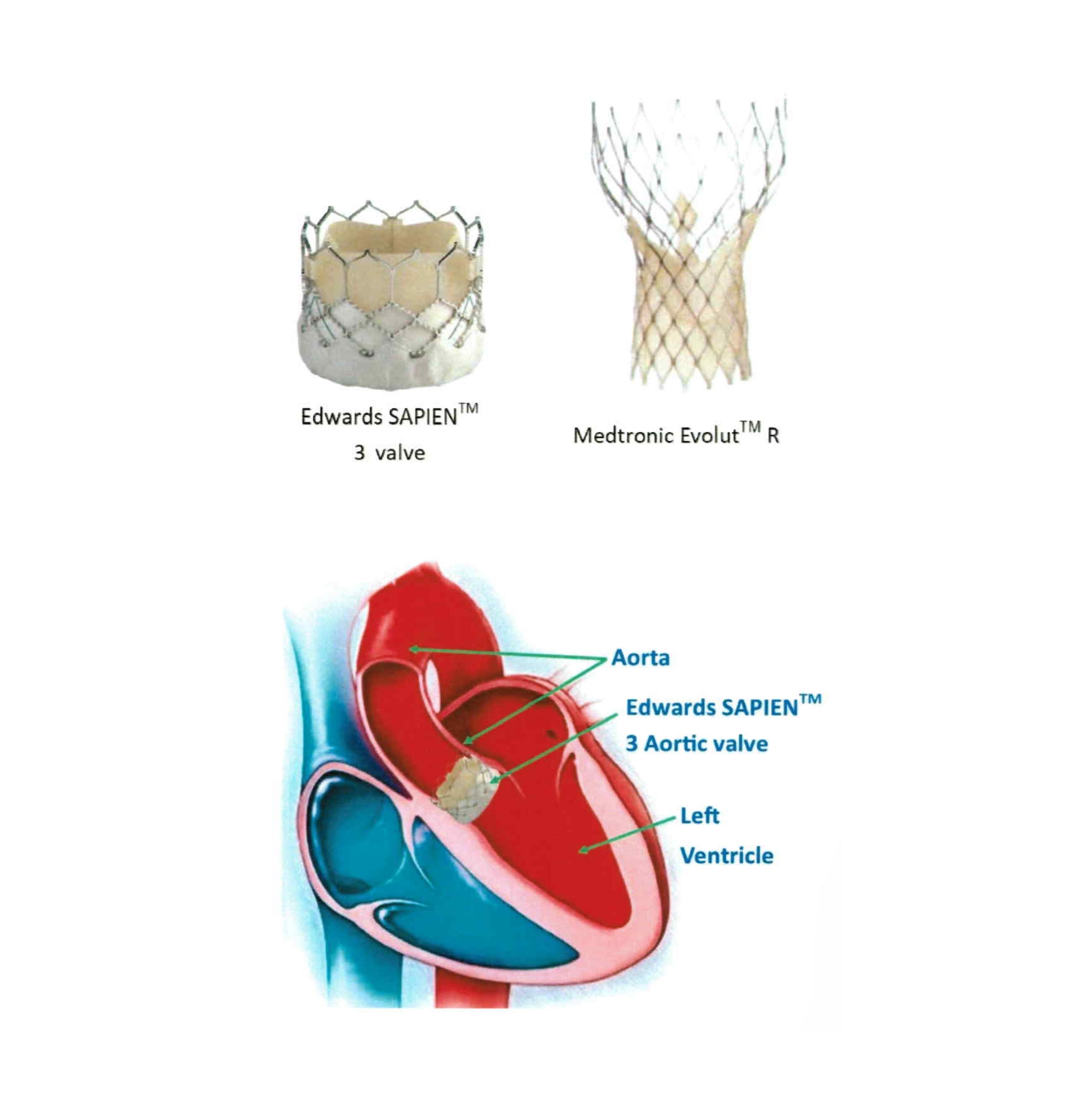
The valve is made out of pig or cow heart tissue and stitched on to a small metal frame (stent). The valve is made to work like the valve you are born with.
The valve is delivered using a balloon catheter system.X-rays and ultrasound are then used to see where the catheters are and check the position of the valve.
Once the valve is in the correct position, the balloon is inflated and the valve is delivered. The frame of the new valve pushes your narrowed valve leaflets against the wall of the aorta. Your new valve uses the plaque on your old valve to keep it in place. Once in position the balloon is deflated and your new valve will start working.
Your TAVI doctor will check that your new valve is working correctly using ultrasound. Once happy the catheters are then removed and the cut in your leg closed using a stitch inside the blood vessel.
After the Procedure
The breathing tube is normally removed.
You will be moved back to your bed and transferred to the Cardiothoracic Intensive Care Unit (ICU) or Coronary Care Unit (CCU) to recover the night of your procedure.
You may still have a tube in your neck for fluids and one in your arm. The urinary catheter may also be in your bladder after the procedure.
As soon as possible we will try to remove as many of the tubes and catheters either the same or next day.
You will need to lie flat for 4 hours after your procedure, we will remind you to keep your legs straight. This is to stop the cuts in your legs from bleeding. The cuts in your groin will be checked by the nurse frequently.
As soon as it is safe the nurses will get you out of bed to sit in the chair and walking around the ward. It is important to start moving and getting back to normal activity as soon as it is safe to do so.
Once you are awake enough you will be allowed to eat and drink.
You will get a Transthoracic Echocardiogram (TTE) to check the valve position the afternoon of your procedure or the next morning. You may also need some blood tests before you leave the hospital.
Avoid activity such as mowing, running or hard labour and do not lift objects more than 5kg (10lbs) for 5 days after your procedure.
Wound Site Care
- The dressing on your wrist or groin can be taken off the day after your procedure.
- You may take a shower the day after your procedure, do not take a bath or go swimming for 2 days after your procedure. Do not scrub the wound site for a week, wash lightly and pat dry. Avoid creams, lotions or ointments to the wound site.
- Notify your nurse or doctor if you notice any of the following:
- A lump that is getting bigger or any swelling at the procedure site
- Constant redness or warmth
- Worsening numbness or discomfort (mild discomfort is normal)
- Yellow ooze/pus from the wound site
- A lump that is getting bigger or any swelling at the procedure site
If there is bleeding or a lump getting bigger at the wound site
1) Lie down straight away and apply firm pressure (enough to feel the heart beat under your fingers) to the site for 15 minutes.
2) If the bleeding continues or is a large uncontrolled amount or you feel faint or dizzy call ‘000’ immediately. Do not drive yourself to the hospital. Continue to apply pressure until help arrives.

Planning To Go Home
You will need to make arrangements with your family and friends to take you home once you are recovered (2-4 days). You will not be able to drive yourself home or take public transport or a taxi.
It is best to plan ahead and make sure you have someone at home with you for the first 1-2 weeks after you leave hospital. If you think that you may have difficulty at home and require some services to assist you such as meals on wheels or cleaning, we can arrange for a social worker to see you.
We will give you a list of all your medications when you leave hospital. We may also give you a prescription for Clopidogrel (Plavix®). Clopidogrel is very important to keep taking as it helps to stop blood clots on your new valve.

Follow Up
Please see your local doctor in 3 days after leaving the hospital.
An appointment will be made for you to follow up with your TAVI Cardiologist at 1 month after the procedure. You will have a Transthoracic Echocardiogram (TTE) to check the valve.
You will need to see your normal Cardiologist at 6 months and 1year for another Transthoracic Echocardiogram (TTE) to check the valve.
You will be referred to cardiac rehab to attend a 6 week program starting 2 weeks after your procedure. One month after your TAVI the rehab team will also do a 6 minute walk test to check your progress after the new valve.