Pacemaker (PPM) Implantation
What is a Pacemaker?
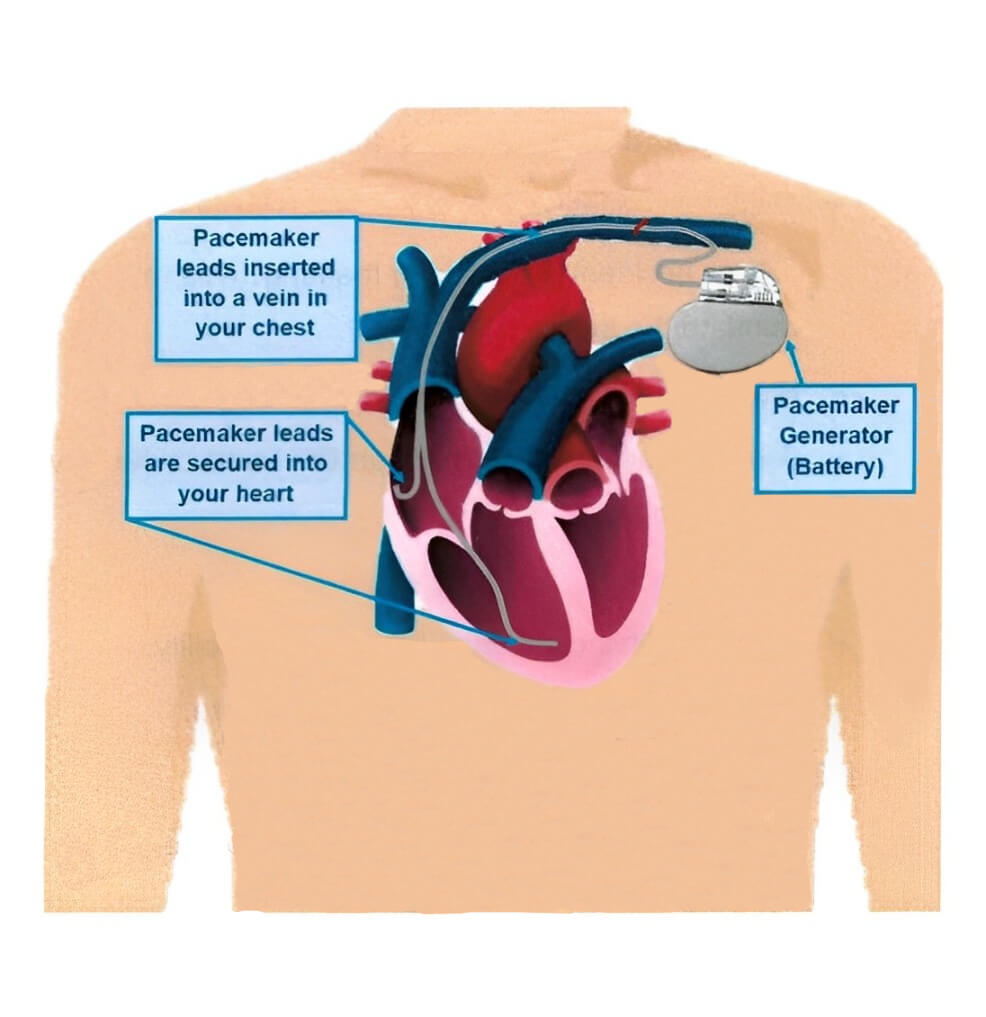
A pacemaker is made up of 2 parts;
- A small generator (battery) that sits underneath your skin.
- Leads (electrodes) that sit inside your heart, connected to the generator.
The pacemaker helps your heart beat properly. The leads sense when your heart is beating too slow and send a signal to the generator. The generator then sends an impulse down the leads to your heart muscle. This impulse allows your heart to beat at the right pace. The pacemaker only works when needed.
Your pacemaker also monitors your heartbeat and stores this information. This allows your doctor to review your heartbeat activity and make changes to your pacemaker settings as needed. Your pacemaker battery will be checked by your doctor at your follow-up visits. The battery lasts between 6 to 8 years. When the battery low and is in need of replacement you will need a similar procedure to replace it. It cannot be recharged.

Why do you need a Pacemaker?
Your heart beats too slow (bradycardia). This can make you feel dizzy, tired, short of breath and have fainting spells (syncope). These put you at risk of injury.
How long will the procedure take?
The whole procedure will take 1 -2 hours to complete.
What are the risks?
Your doctor has recommended you for a pacemaker as they believe the overall benefits to you outweigh the risk of not going ahead with the procedure. There are risks and complications related to this procedure. They include but are not limited to the following.
- Minor or Major bruising or swelling at the pacemaker puncture site.
- The pacemaker lead may move or the battery may fail. This may need to be replaced by repeating the procedure.
- Infection at the site of the pacemaker. This may need treatment with antibiotics or removal of the pacemaker/pacemaker leads.
- A higher lifetime risk of cancer from x-ray exposure.
- A hole accidentally made in the lung. This may need a tube to be placed into your lung to reinflate the lung.
- Blood clot in the subclavian vein or lungs.
- A hole is accidentally made in the heart or heart valve. This may need emergency heart surgery to fix.
- Heart attack.
- A stroke. This can cause long term disability.
- Death as a result of this procedure is rare.
Before Your Procedure
Do not eat anything 6 hours before your procedure. You may drink only clear fluids up until 2 hours before your procedure.
If you are diabetic and take Metformin (Diabex®, Diaformin®) stop taking 2 days before and 2 days after your procedure. If you take Empagliflozin or Dapagliflozin (Forxiga®, Xigduo XR®, Jardiance®, Jardiamet®, Glyxambi® or Qtern®) stop taking 3 days before your procedure.
Please let us know if you are allergic to lodine, Contrast or any other medications.
Please arrange a friend or family member to take you home from hospital and stay with you for your first night at home. You cannot go home alone or in a taxi.
Ask any questions that you or your family may have and sign a form consenting to the procedure.
You will be asked to change into a hospital gown. An ID band will be applied. Your procedure site (chest) clipped of any hair. The healthcare team will take your vital signs (blood pressure and pulse) and insert an IV (intravenous) line into a vein in your arm.
Your Cardiologist may stop your Rivaroxaban & Apixaban 2-3 days before the procedure. Aspirin, Clopidogrel, Prasugrel & Ticagrelor are usually continued.
You will be given antibiotics before your procedure. This is to help stop an infection.
During the Procedure
- A heart tracing (ECG) is placed on your chest, a blood pressure sleeve on your arm and you are monitored the whole time during the procedure.
- You will be given sedation and analgesia either by the anaesthetist or nurse to make you comfortable during the procedure. You may have an oxygen mask on your face. If you have a general anaesthetic, once you are asleep a breathing tube will be put into your trachea (wind pipe) and you will be connected to a ventilator (breathing machine) for the procedure. If you have sedation you will be able to breathe on your own but be made sleepy and relaxed during the procedure. A nurse will be available to assist you if you have any concerns during your procedure.


- Your chest will be cleaned with antiseptic solution and you will be covered with a drape.
Local anaesthetic is injected to the area below your left or right collarbone. This will then become numb. - Once the area is numb the doctor will make a small incision just under your collarbone.
- The pacemaker lead is then placed in your heart by inserting the lead through a vein in your chest. This is done using x-rays.
- Once the leads are in place they will be connected to the generator (battery). The generator is then placed just under the skin. Your incisions is then closed with stitches, these will dissolve and do not need to be removed. A dressing will be placed over the wound.
After the Procedure
After the procedure you will be taken back to the ward. You will need to stay in bed for a few hours afterwards to wake up from the sedation/anaesthetic. If you have pain please let your healthcare team know. You may eat and drink on return to the ward.
You will need to stay overnight, have a chest x-ray and device check before you can go home.
You should be moving the arm on the same side as the wound up to shoulder height to avoid stiffness. Do not raise this arm above shoulder height. Avoid lifting anything weighing more than 5kg (10lbs) for 4 weeks.
You can use all household items, but should avoid those with magnets and strong electric fields. You may use a mobile phone on the opposite side to your implanted device.
Wound Site Care
- If a dressing is applied the day after your procedure it should be left in place for 5 days and then removed. Keep the dressing dry.
- Do not apply any creams, lotions or powders to the wound site until fully healed.
- Try not to rub, scratch or itch the site until fully healed.
- Avoid wearing clothing that will rub on the wound for 2-3 weeks
- You may require additional padding between a seatbelt and your wound.
- If you are given a course of antibiotics it is important to complete the course to reduce the risk of infection.
- You may take a shower the day after your procedure. Do not take a bath or go swimming for 2 weeks after your procedure. Do not scrub the wound site, lightly wash and pat dry.
- Notify your nurse or doctor if you notice any of the following:
- A lump that is getting bigger or any swelling
- Constant redness or warmth
- Worsening numbness or discomfort (mild discomfort is normal)
- Yellow ooze/pus from the wound site
- Chills or fever
- A lump that is getting bigger or any swelling
Security Systems At The Airport And Your Device
The system may detect your device and set off the alarm. It will not affect the functioning of your device.
Show your device ID card to the security personnel. Ask that they not use the handheld screening wand because it might affect your device.


Driving once you are home
- Do not drive for at least 2 weeks after your procedure. If you have had a heart attack or drive a commercial vehicle this may be longer (2-4 weeks).
- Your Cardiologist or the Roads and Maritime Service can provide more information.
Follow Up
- Please see your local doctor in 3 days and make an appointment to see your Cardiologist in 4 weeks.
- An appointment may be made for you to follow up in a week at the cardiac diagnostics unit for a device and wound check. Please confirm appointment details with your healthcare team before leaving hospital.