Pulmonary Vein Isolation
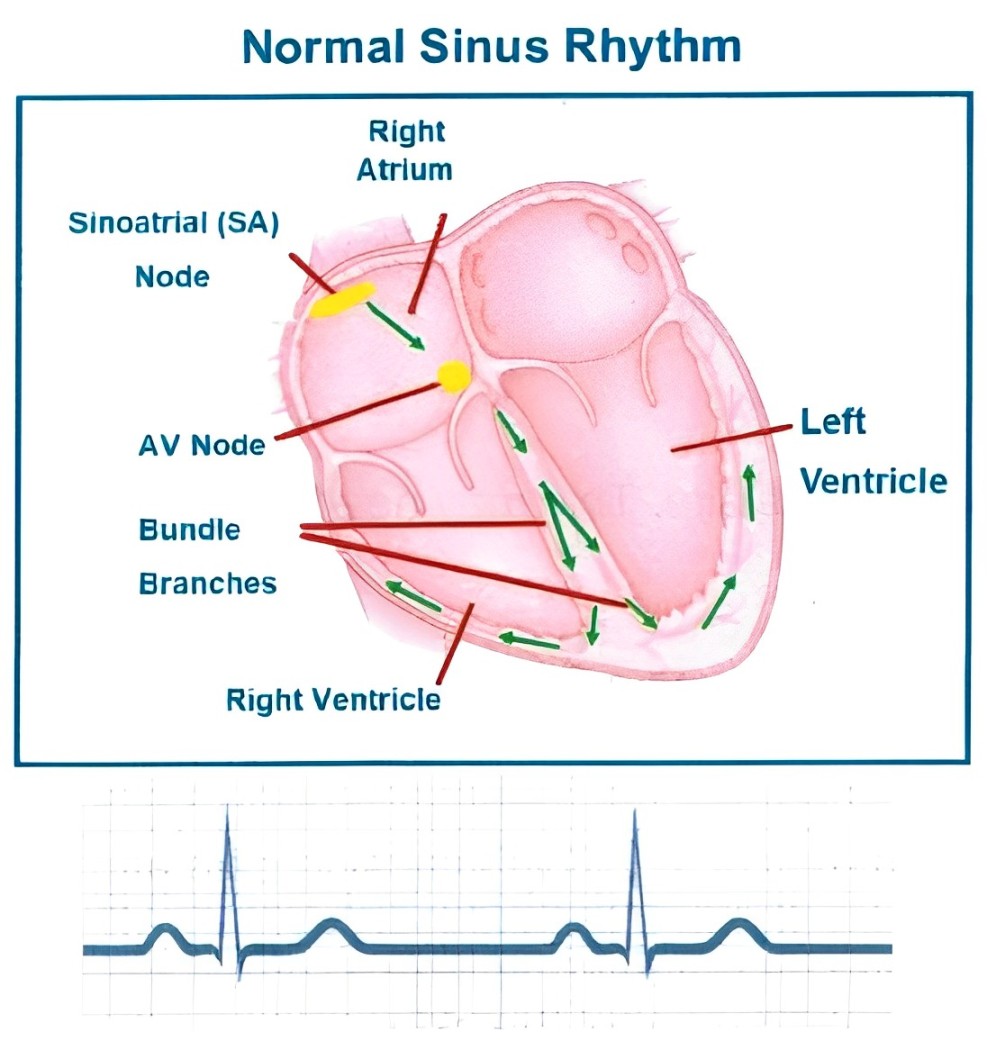
The Normal Electrical System of the Heart
The heart has 4 chambers, 2 atria (upper) and 2 ventricles (lower). Your heartbeat starts by a group of cells called the sinoatrial or sinus (SA) node in the right atrium. The electrical impulse then spreads from the atria (upper chambers) causing them to contract and pump blood into the ventricles (lower chambers). The impulse then spreads to the AV node. This slows down and controls the impulses between the atria and ventricles. From the AV node the impulse travels down the bundle branches to allow the ventricles to contract and pump blood around the body.
The Heart During Atrial Fibrillation
In Atrial Fibrillation (AF) your heartbeat does not start at the SA node. Instead many impulses start and spread chaotically throughout the atria. The atria are then not able to contract and pump blood to the ventricles and instead they fibrillate (tremble). The electrical impulse then spreads to the ventricles in a chaotic way. This causes them to contract irregularly and at times faster than normal. This can lead to the ventricles not being able to pump enough blood to the body. This can at times make you to feel short of breath, have palpitations or get light headed.
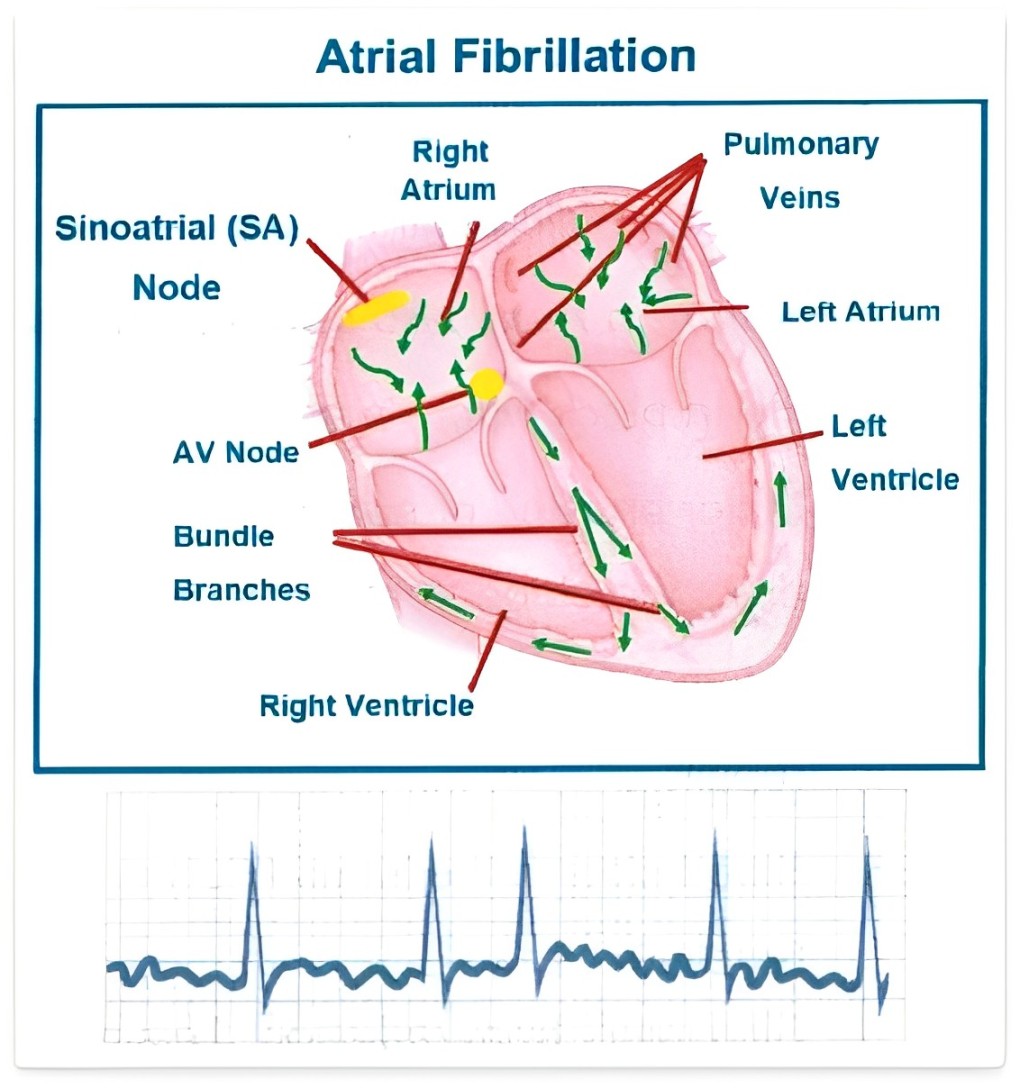
What is a Pulmonary Vein Isolation (PVI)?
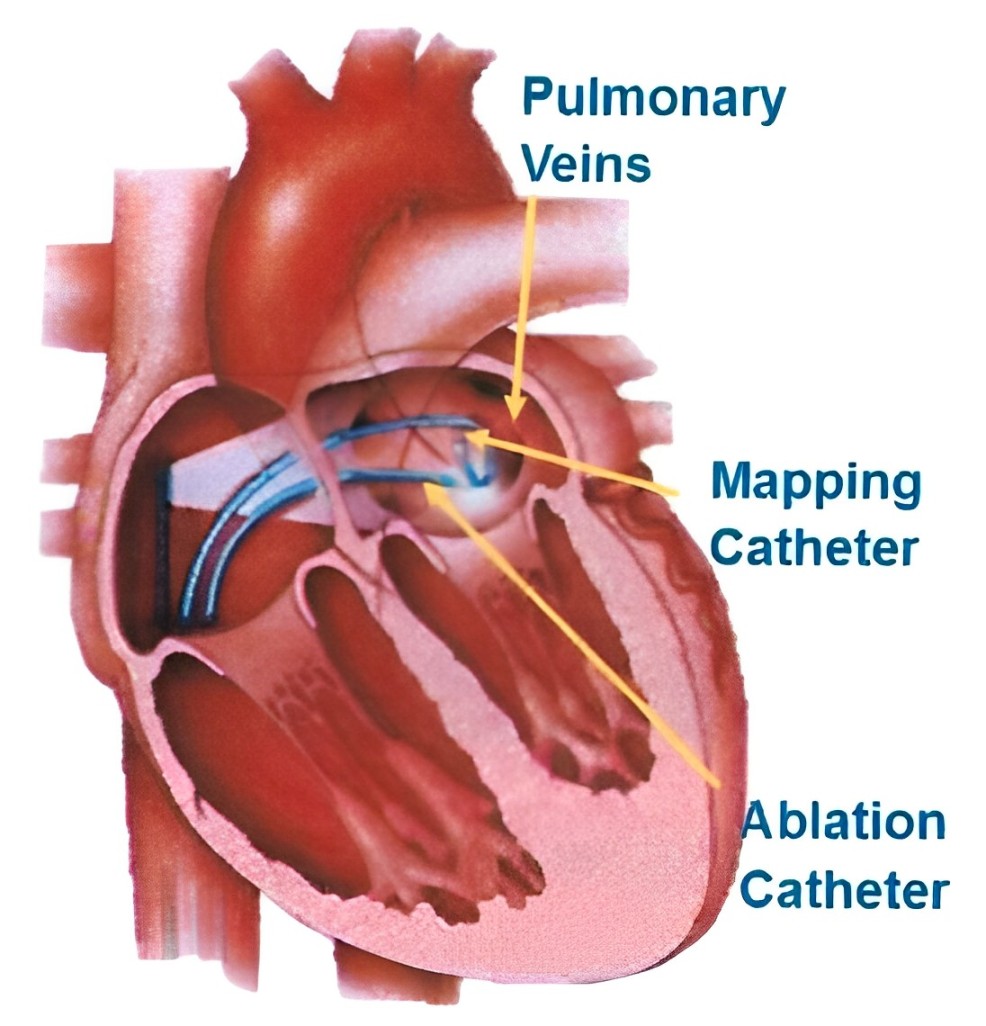
There are 4 pulmonary veins that drain blood from your lungs back into your heart. The pulmonary veins are also where extra electrical impulses that cause AF can start. PVI is a type of cardiac ablation used to treat AF that has not been able to be treated with medications.
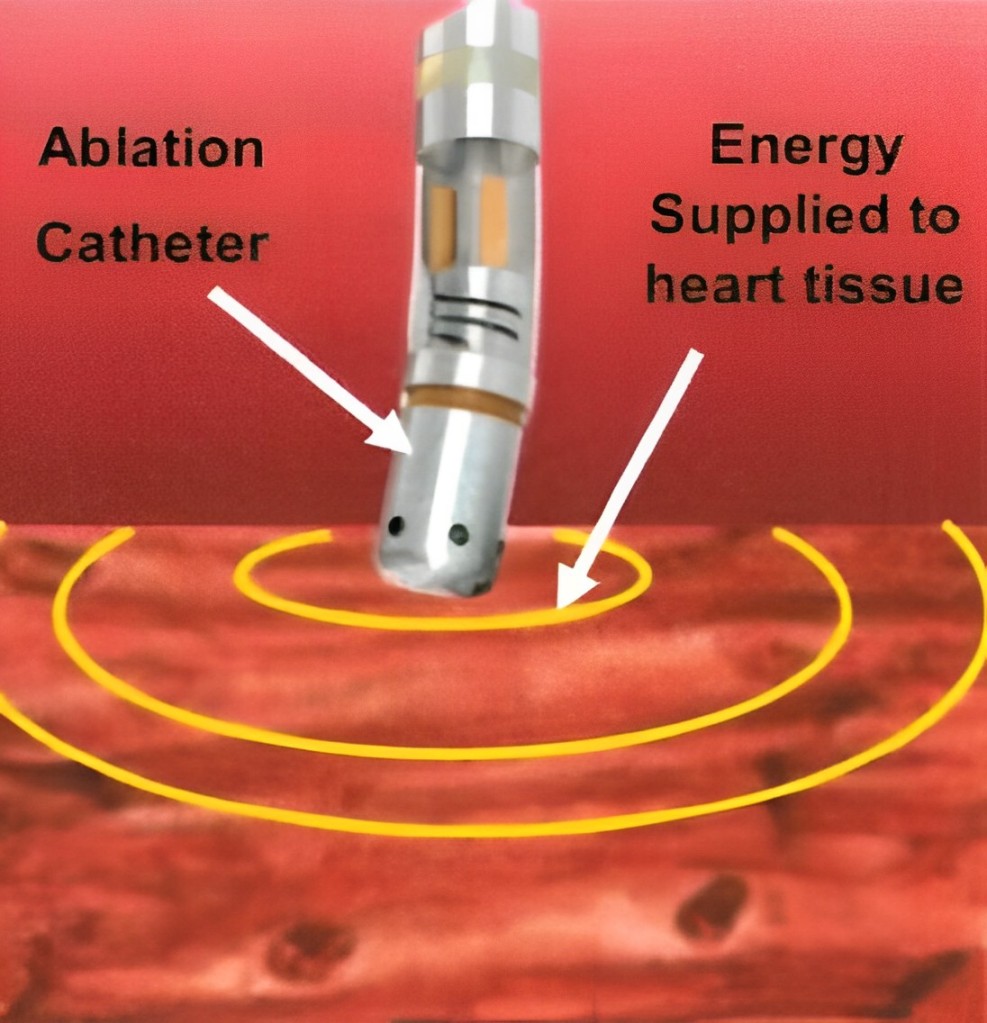
The doctor applies energy, radiofrequency (heat) or Cryo (cold), to your heart tissue. This creates a scar that blocks the electrical signals coming from the pulmonary veins. This is repeated around the entrance to all 4 pulmonary veins.
What are the risks?
Your doctor hasrecommended you for a Pulmonary Vein Isolation as they believe the overall benefits to yououtweigh the risk of not going ahead with the procedure. There are risks andcomplications related to this procedure. They include but are not limited to the following.
Minor bruising at the puncture site.
Heart block where a pacemaker may be needed.
Major bruising or swelling at the groin puncture site. This may need surgery to drain the blood from the bruise.
A hole is accidentally made in the heart or heart valve. This will need surgery to repair.
Blood clots in the lungs (Pulmonary embolism) or leg (DVT) causing pain and swelling.
Skin injury from radiation. This may cause reddening of the skin.
Accidental tear/puncture of the artery. This may need surgery to fix.
A higher lifetime risk from exposure to radiation.
A stroke. This may cause long term disability.
A punctured lung. This may need a tube to be put in to the chest to reinflate the lung.
Heart attack.
Death as a result of this procedure is rare.
Before Your Procedure
If you are diabetic and take Metformin (Diabex®, Diaformin®) stop taking 2 days before and 2 days after your procedure. If you take Empagliflozin or Dapagliflozin (Forxiga®, Xigduo XR®, Jardiance®, Jardiamet®, Glyxambi® or Qtern®) stop taking 3 days before.
Please let us know if you are allergic to lodine, contrast or any other medications.
You may be asked to stop taking Rivaroxaban or Apixaban and switch to another blood thinning medication such as Warfarin or Dabigatran.
Continue to take all your medications unless instructed by your Cardiologist.
Do not eat anything 6 hours before your procedure and only drink clear fluids until 2 hours before your procedure.
You may be asked to have a CT scan to further evaluate your heart anatomy before your procedure date. It is important that you attend this appointment.
Please arrange a friend or family member to take you home from hospital and stay with you for your first night at home. You cannot go home alone or in a taxi.
You will change into a hospital gown, be given an ID armband and your groin clipped of any hair. Your healthcare team will take your vital signs (blood pressure and pulse) and insert an IV (intravenous) line into a vein in your arm.
Ask any questions that you or your family may have and sign a form consenting to the procedure.
During the Procedure

The procedure is done in a Cardiac Catheterisation Laboratory (Cath Lab) that looks like an operating theatre. You will lie on a narrow x-ray table flat on your back. It is a sterile lab and the staff will be wearing gowns, masks and caps. A heart tracing (ECG) is put your chest, a blood pressure sleeve on your arm and monitored during the procedure.
Cold gel patches will be placed on your chest and back.
The Anaesthetist will give you medications to make you fall asleep. You may have an oxygen mask on your face. Once you are asleep a breathing tube will be put into your trachea (wind pipe) and you will be connected to a ventilator (breathing machine) for the procedure.
A Transoesphageal Echocardiograph (TOE) is done to look at the chambers of the heart and check for blood clots. If there are blood clots the procedure will not continue and you will be woken up.
Your groin will be cleaned with antiseptic solution and you will be covered with a drape.
Catheters (tubes) the size of a small drinking straw are then placed inside your heart. A small hole is made with a needle (transeptal puncture) to cross from the right side of your heart to the left. This is done under x-ray to get to the pulmonary veins.
Energy is then supplied to the pulmonary veins to create a scar to stop the abnormal electrical activity.
During procedure you will be asleep and should not feel any discomfort.
How long will the procedure take
The procedure will take 2 1/2 -4 hours.
After the Procedure
When the procedure is over the catheters (tubes) are removed. The incision is closed by pressing firmly on the site. You will be woken up and taken to the recovery unit. You will return to the ward where you will stay overnight until you are discharged.
Activity After the Procedure & At Home
Rest on the day of your procedure.
Slowly return to normal activities and full activity/work after a week.
Avoid strenuous activity such as running or hard labour for 5 days afterwards.
Limit stair climbing as much as possible on the day of your procedure.
Do not lift objects more than 10kg (20lbs) for 7 days after your procedure.
Do not drive for at least 2 days after your procedure. You should also not drive if there are any other symptoms that may affect your ability to control a vehicle.
Do not stop or change any of your medications unless instructed by your Cardiologist.
Wound Site Care
The dressing on your groin can be removed the day after your procedure.
You may take a shower the day after your procedure. Do not take a bath or go swimming for 7 days following your procedure.
Notify your nurse or doctor if you notice any of the following:
Worsening numbness or discomfort
(mild discomfort is normal)
· A lump that is getting bigger
. Constant redness or warmth
. Yellow ooze/pus from the wound site

If there is bleeding or a lump getting bigger at the wound site
1) Lie down and apply firm pressure to the site for 10 minutes.
2) If bleeding continues or is a large uncontrolled amount call ‘000’ immediately. Do not drive yourself to the hospital.
3) Continue to apply pressure until help arrives.
What to do if you experience any chest discomfort
Chest pain occurs in 1 out of 3 people after a PVI.
It is usually an aching sensation in the centre of the front of the chest but may be worse with deep breathing. If the pain is severe after the procedure you may be kept in hospital longer. If it is not severe you may go home but sometimes the pain worsens after going home.
If you get mild to moderate pain at home you can take paracetamol or codeine.
Avoid other anti-inflammatory medications (Nurofen® or Ibuprofen for example).
If the pain is severe you should go to hospital for assessment. If the pain doesn’t resolve within 72 hrs let your cardiologist know and see your local doctor.


Other symptoms to look out for
You may have a night sweat the night after the procedure and again the next night. If this continues or if you develop fevers more than 72 hours after the procedure you should alert your cardiologist and see your local doctor.
If you have severe shortness of breath, severe dizziness or collapse call ‘000’ immediately. Do not drive yourself to the hospital.
For other unexpected symptoms please see your local doctor and inform your cardiologist. If the symptoms are severe call ‘000’ immediately.
Do not drive yourself to the hospital.
Follow Up
Please see your local doctor in 3 days and make an appointment to see your cardiologist in 4 weeks after leaving the hospital.
Recurrence of the Abnormal Heart Rhythm
It is not unusual to have an abnormal heart rhythm after a PVI. This may be due to the healing process and may settle down with time. Sometimes it may continue and you may need a 2nd procedure to fix the problem. If it occurs within 3 months of the procedure we recommend you try to get an ECG to show the abnormal heart rhythm. Your local doctor may be able to arrange one and send it through to your cardiologist. It is helpful to let your cardiologist know about these symptoms.