Left Atrial Appendage Closure
What is the left atrial appendage closure?
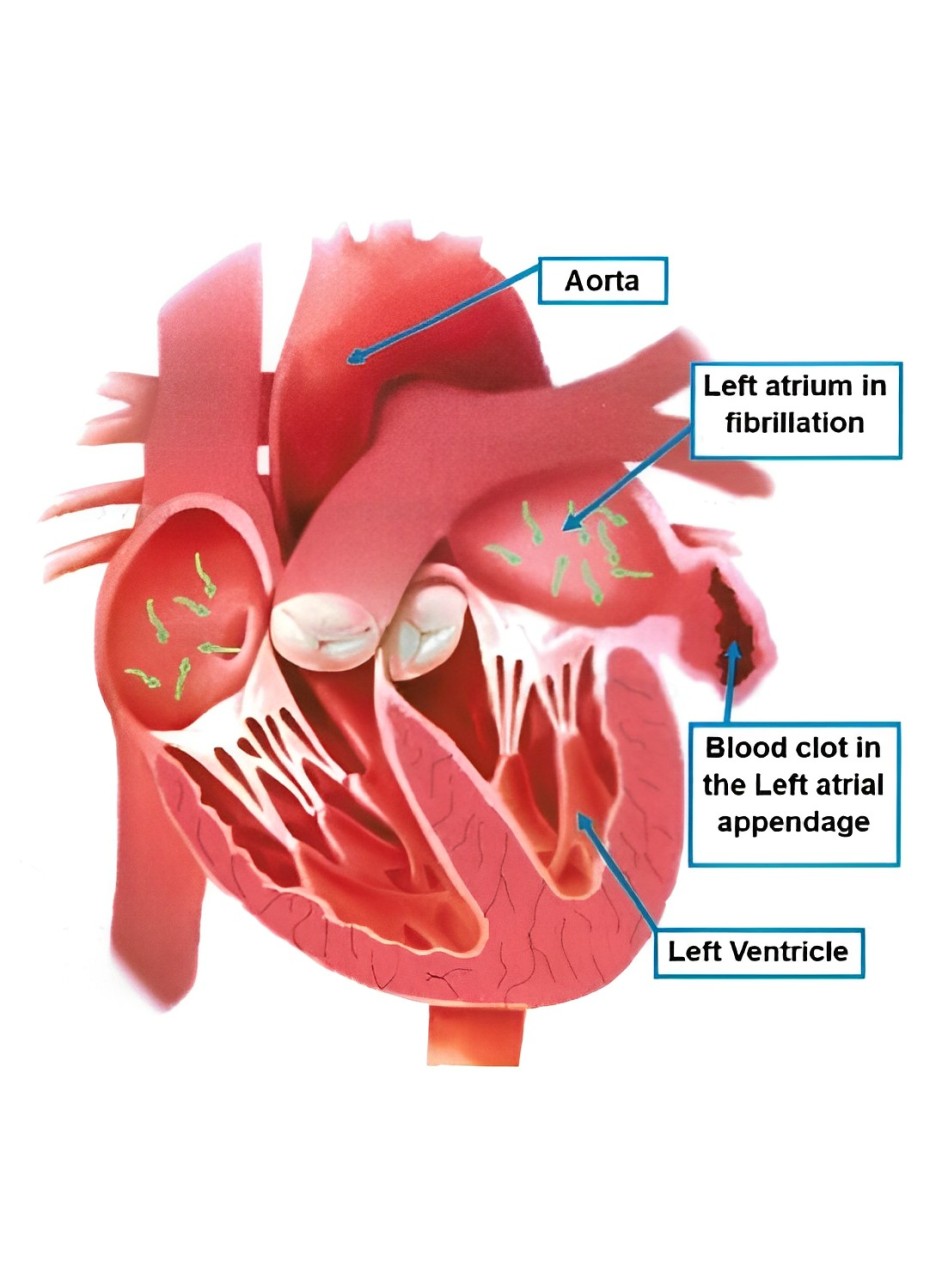
The heart has 4 chambers, 2 upper (atria) and 2 lower (ventricles).
The left atrial appendage (LAA) is a small pouch in the muscle wall of the left atrium of the heart.
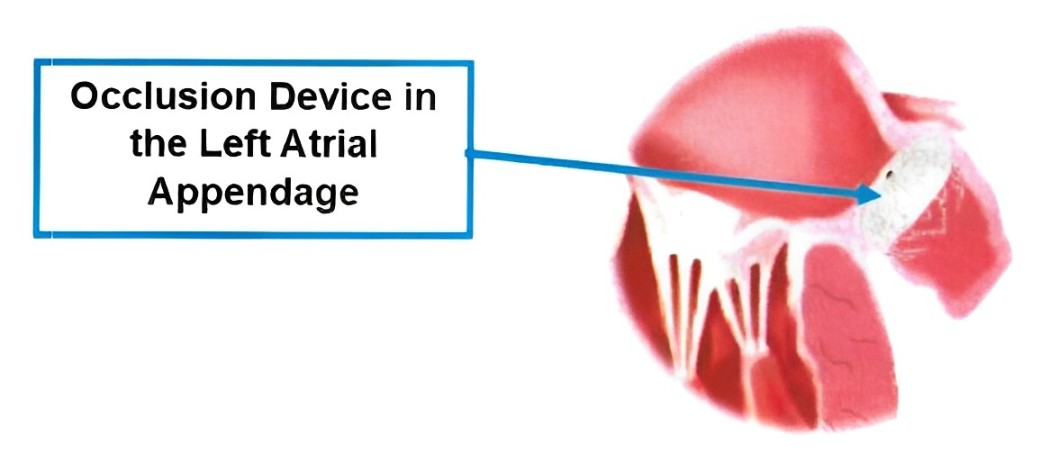
A left atrial appendage closure is a procedure which closes off this pouch.
Your doctor may recommend this procedure if you have a condition known as atrial fibrillation (AF), where your heart’s electrical system is disturbed and your heartbeat becomes irregular and unco-ordinated.
Normally, with each heartbeat, blood is pumped out of the top chamber (left atrium) into the bottom chamber (left ventricle) and then to the rest of your body.
If you have AF blood can’t be squeezed out of your left atrium properly, and it can collect and clot in your LAA increasing your chances of having a stroke.
Blood thinning medications such as Warfarin are usually given to treat AF but they aren’t suitable for everyone. If you can’t take this medication, your doctor will recommend a procedure to close the opening of the LAA to prevent clots traveling to your brain.
What are the risks?
Your doctor has recommended a Left Atrial Appendage Closure as they believe the overall benefits to you outweigh the risk of not going ahead with the procedure. There are risks and complications related to this procedure. They include but are not limited to the following.
Minor bruising at the puncture site.
Major bruising or swelling at the groin puncture site. This may need surgery to drain the blood from the bruise.
A hole is accidentally made in the heart or heart valve. This will need surgery to repair.
Blood clots in the lungs (Pulmonary embolism) or leg (DVT) causing pain and swelling.
Abnormal heart rhythm that may need an electric shock to correct.
Infection, this may need treatment with antibiotics.
Incomplete closure of the left atrial appendage
Allergic reaction to the device and medications
Bleeding that may need emergency surgery or a blood transfusion to fix.
A stroke. This may cause long term disability.
Death from this procedure is rare.
Check that everything is working
See if the signal quality is good and the stickers are still OK
See how much longer your monitoring has to go
Before Your Procedure
Do not eat anything 6 hours before your procedure, you may drink only clear fluids up until 2 hours before your procedure.
Do not smoke or drink alcohol the day before, or on the day of your procedure.
Please arrange a friend or family member to take you home from hospital and stay with you for your first night at home. You cannot go home alone or in a taxi.
If you are diabetic and take Metformin (Diabex®, Diaformin®) stop taking it 2 days before and 2 days after your procedure.
If you are diabetic and take Empagliflozin (Glyxambi®, Jardiamet®, Jardiance®) or Dapagliflozin (Forxiga®, Xigduo XR®, Qtern®) you must stop taking it 3 days before your procedure.
Your Cardiologist may stop your Warfarin, Dabigatran (Pradaxa®), Rivaroxaban (Xarelto®) & Apixaban (Eliquis®) 2 days before your procedure.
Aspirin, Clopidogrel (Plavix®), Ticagrelor (Brilinta®) and Prasugrel (Effient®) need to be continued.
Please let us know if you are allergic to lodine, contrast or any other medications.
Ask any questions that you or your family may have and sign a form consenting to the procedure.
You will change into a hospital gown, an ID band will be applied and your groin clipped of any hair. The healthcare team will take your blood pressure and pulse and insert an IV (intravenous) line into a vein in your arm.
During the Procedure
Your procedure is done in the Cardiac Catheterisation Laboratory (Cath lab) that looks like an operating theatre. It is a sterile lab and the staff will be wearing gowns, masks and caps. You will lie on a narrow x-ray table flat on your back. Small adhesive dots are placed on your chest (ECG) and a blood pressure sleeve on your arm, these are used to monitor you during the procedure.
The Anaesthetist (doctor) will give you medications to make you fall asleep. You may have an oxygen mask on your face. Once you are asleep a breathing tube will be placed in your trachea (wind pipe) and you will be connected to a ventilator (breathing machine) for the procedure.
Once you are asleep a probe is placed into your food pipe (oesophagus) to look at the chambers of the heart and check for blood clots. If there are clots the procedure will not continue and you will be woken up.
Your groin will be cleaned with antiseptic solution and you will be covered with a drape.
A catheter (long thin hollow tube) is placed inside your heart. A small hole is made with a needle (transeptal puncture) to cross from the right upper chamber to the left. X-ray is then used to help deliver and position the closure device in the LAA.

How long does the procedure take?
This procedure usually takes 2 – 3 hours.
After the Procedure
When the procedure is finished the catheters (tubes) are removed. The incision in your groin is closed by a nurse or doctor pressing firmly on the site.
You will be woken up and taken to the recovery room. When the anaesthetic wears off you will be transferred back to the ward where you will stay overnight until discharge.
You will have to lie flat for several hours after the procedure to reduce the risk of bleeding from the procedure site in the groin.
The nurses on the ward will let you know when you can sit up and when you can eat and drink again.
Your doctor will explain the results of the procedure.
Rest on the day of your procedure.
Slowly return to normal activities and full activity/work after a week.
Avoid strenuous activity such as running or hard labour for 5 days afterwards.
Limit stair climbing as much as possible on the day of your procedure.
Do not lift objects more than 10kg (20lbs) for 7 days after your procedure.
Do not drive for at least 2 days after your procedure, or
if you have any other symptoms that may affect your ability to control a vehicle.
Do not stop or change any of your medications unless instructed by your Cardiologist.
Wound Site Care
The dressing on your groin can be removed the day after your procedure.
You may take a shower the day after your procedure but do not take a bath or go swimming for 7 days after your procedure. Do not scrub the wound site for a week, lightly wash it and pat dry. Avoid creams, lotions or ointments to the wound site.
Notify your doctor or come to the emergency department if you notice any of the following at the wound site:
Worsening numbness or discomfort (mild discomfort is normal)
A lump that is getting bigger
Constant redness or warmth
Yellow ooze/pus from the wound site

If there is bleeding or a lump getting bigger at the wound site
1) Lie down straight away and apply firm pressure (enough to feel the heart beat under your fingers) to the site for 10 minutes.
2) If bleeding continues or is a large uncontrolled amount or you feel faint or dizzy call ‘000’ immediately. Do not drive yourself to the hospital.
3) Continue to apply pressure until help arrives.
Follow Up
Please see your local doctor in 3 days and make an appointment to see your Cardiologist within 4 weeks after leaving the hospital.