Coronary Angiography
A Coronary Angiogram is done if you have the following:
Symptoms of chest pain
Abnormal results on a test such as Echocardiograph, Exercise Stress (treadmill) Test, Sestamibi Scan, Electrocardiograph (ECG) or Computed Tomography Coronary Angiography (CTCA)
Aheart valve problem that requires surgery or organ transplant surgery
Aheart defect you were born with
Other blood vessel problems or a chest injury
A Coronary Angiogram is done if you have the following:
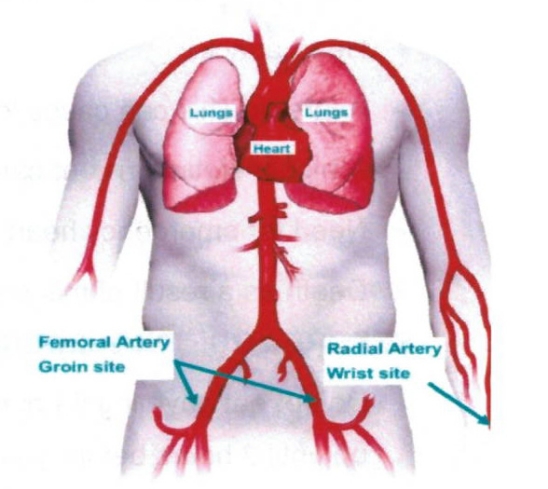
A coronary angiogram checks for any blockages/ narrowing of the blood vessels (arteries) of your heart. You will be injected with a numbing medication (local anaesthetic). A thin flexible tube (catheter) is inserted into a blood vessel (artery) in either your groin (femoral) or your wrist (radial).
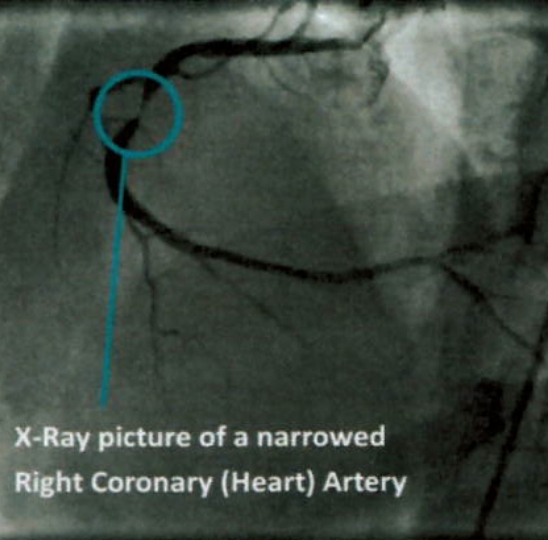
You may also be given medication to make you sleepy and relaxed (sedation). Once the tube is in position, contrast dye is injected. An X-ray machine will move over you, very close to your body and x-ray pictures are taken of the blood vessels of your heart (coronary arteries). These pictures will show any narrowing or blockages, caused by plaque (fatty) X-Ray picture of a narrowed Right Coronary (Heart) Artery deposits. During the angiogram the pumping function of the heart (left ventricle) and the heart valves may also be checked. During this part of the procedure you may feel warm all over your body or the urge to go to the toilet as the dye is injected. Do not worry this is normal and will pass in a 10-15 seconds after flowing around your body.
How long will it take?
Approximately 30 minutes to 90 Minutes.
What are the risks?
Your doctor has recommended you for a Coronary Angiogram as they believe the overall benefits to you outweigh the risk of not going ahead with the procedure. There are risks and complications related to this procedure. They include but are not limited to the following.
- Loss of pulse in the arm after a radial artery (arm) procedure.
- Minor or Major bruising or swelling at the groin/arm puncture site.
- Abnormal heart rhythm that may need an electric shock to correct.
- Surgical repair of the groin/arm puncture site or blood vessel.
- Loss of kidney function due to the side effects of the contrast dye.
- Heart attack.
- Astroke. This can cause long term disability.
- Ahigher lifetime risk of cancer from x-ray exposure.
- Need for emergency heart surgery or angioplasty.
- Death as a result of this procedure is rare.
Before Your Procedure
Do not eat anything 6 hours before your procedure, you may drink only clear fluids up until 2 hours before your procedure.
If you are diabetic and take Metformin (Diabex®,Janumet®, Diaformin®) stop taking 2 days before and 2 days after your procedure. If you take Empagliflozin or Dapagliflozin (Forxiga®, Xigduo XR®, Jardiance®, Jardiamet®, Glyxambi® or Qtern®) stop taking 3 days before.
Please let us know if you are allergic to lodine, Contrast or any other medications.
Please arrange a friend or family member to take you home from hospital and stay with you for your first night at home. You cannot go home alone or in a taxi.
You will change into a hospital gown, be given an ID armband and your groin and wrist clipped of any hair. Your healthcare team will take your vital signs (blood pressure and pulse) and insert an IV (intravenous) line into a vein in your arm.
ASK any questions that you or your family may have and signa form consenting to the procedure
Your Cardiologist may stop your Warfarin, Dabigatran, Rivaroxaban & Apixaban 2-3 days before the procedure, however Aspirin, Clopidogrel, & Ticagrelor are usually continued.
During the Procedure

The procedure is done in a Cardiac Catheterisation Laboratory (Cath Lab) that looks like an operating theatre. You will lie on a narrow x-ray table flat on your back, the table may move from side to side during the procedure. It is a sterile lab and the staff will be wearing gowns, masks and caps. A heart tracing (ECG) is placed on your chest and monitored the whole time during the procedure. Your groin and/or wrist will be cleaned with a cold antiseptic solution and then you will be covered with a drape. It is important that you try and stay still under the drape. After the local anaesthetic is injected your groin or wrist will become numb and the procedure will begin.
Depending on what your doctor finds during your procedure, you may have another catheter procedure such as a balloon angioplasty or a stent placement to open up a narrowed artery.
After the Procedure
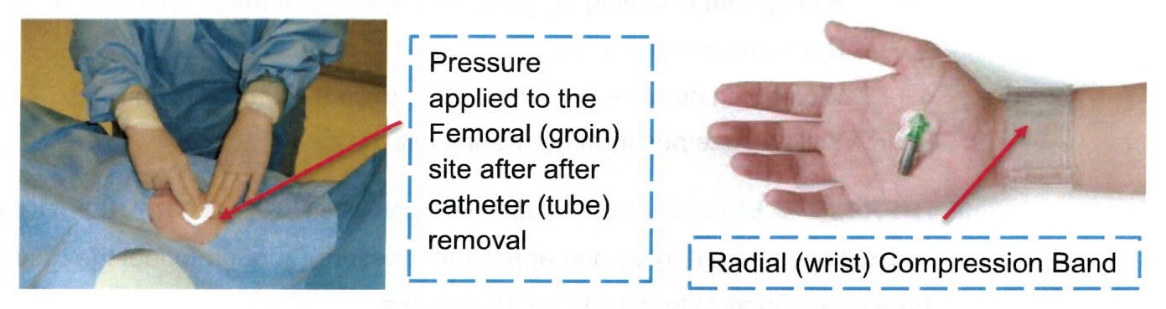
The catheters (tubes) will be removed and the incision closed by pressing on the site, use of a stitch/plug or by placing a band around your wrist to apply pressure. Your doctor will explain the results of the procedure and recommend the best treatment for you. You will return to the ward where you will stay until you are discharged.
Activity After the Procedure & At Home
Rest on the day of your procedure in a bed or recliner chair.
Avoid activity such as mowing, running or hard labour and do not lift objects more than 5kg (10lbs) for 5 days afterwards. Slowly return to normal activities the next day.
Limit stair climbing as much as possible on the day of your procedure.
Limit the use of the affected limb (arm or leg) for the next 48 hours such as using a phone, eating with that arm, typing, bending or squatting.

Driving once you are home
- Do not drive for at least 2 days after your procedure.
- If you have had a heart attack or drive a commercial vehicle this may be longer (2-4 weeks).
- More information can be obtained from your Cardiologist or the Roads and Maritime Services.
Follow Up
Please see your local doctor in 3 days and make an appointment to see your Cardiologist in 4 weeks.
Wound Site Care
- The dressing on your wrist or groin can be taken off the day after your procedure.
- You may take a shower the day after your procedure, do not take a bath or go swimming for 2 days after your procedure. Do not scrub the wound site for a week, wash lightly and pat dry. Avoid creams, lotions or ointments to the wound site.
- Notify your nurse or doctor if you notice any of the following:
A lump that is getting bigger or any swelling at the procedure site
Constant redness or warmth
Worsening numbness or discomfort (mild discomfort is normal)
Yellow ooze/pus from the wound site
If there is bleeding or a lump getting bigger at the wound site
1) Lie down straight away and apply firm pressure (enough to feel the heart beat under your fingers) to the site for 15 minutes.
2) If the bleeding continues or is a large uncontrolled amount or you feel faint or dizzy call ‘000’ immediately. Do not drive yourself to the hospital. Continue to apply pressure until help arrives.

What To Do If You Experience Any Chest Discomfort
If it is travelling to your shoulder, arm, neck or jaw, crushing weight or pressure and combined with any sweating, shortness of breath, nausea or fear.
At the first sign of discomfort
Stop immediately and rest
If no relief with rest
Take 1st nitroglycerine (GTN) tablet or spray
If no relief within 5 minutes
Take 2nd nitroglycerine (GTN) tablet or spray
If no relief after 5 minutes
Call an ambulance ‘000’ and take 3rd nitroglycerine (GTN) tablet or spray
Notify your GP or Cardiologist you have any pain that is relieved by nitroglycerine (GTN) tablet or spray,
**GTN belongs to a group of medicines called nitrates. It lets more blood and oxygen reach the heart muscle.