Transoesophageal Echocardiogram (TOE)

What Is A Transoesophageal Echocardiogram (TOE)?
During a TOE procedure a probe with a transducer (microphone) is put in your mouth and down your oesophagus (food pipe). The probe sends ultrasound waves (echoes) through your heart. These ultrasound waves are then sent to a computer to form an image of your heart chambers, aorta (major blood vessel from the heart) and valves. The images from a TOE are a lot clearer as the oesophagus (food pipe) is close to the heart.
How long will it take?
Approximately 30 minutes.
Why do I need a Transoesophageal Echocardiogram (TOE)?
Your doctor may recommend you for a TOE to exclude:
Blood clots that can form in your heart and then break free allowing the clots to flow to other parts of your body. This can sometimes cause a stroke.
An Infection of the heart, the heart valves or the sac that surrounds the heart.
Heart valve stenosis (a narrowing that blocks blood flow) or regurgitation (a floppy valve causing blood to leak backwards across the valve).
Heart failure or Cardiomyopathy (weak or thickened heart muscle that can lead to poor blood pumping from your heart).
Congenital heart disease. This happens when the heart is not formed correctly as foetus (baby). This can affect blood flow of the heart.
A tumour of the heart.
Dissection (tear) in the wall of the aorta (major blood vessel).
An aneurysm (weakening and bulging) of part of your heart muscle or aorta.
During heart surgery to check how your heart is working and position of any new valves or prosthetics.

What are the risks?
Your doctor has recommended you for a transoesophageal echocardiogram (TOE) as nthey believe the benefits to you outweigh the risk of not going ahead with the procedure. There are risks and complications related to this procedure. They include but are not limited to the following.
Sore throat for 1-2 days after the procedure
Damage to your teeth or jaw because of the TOE probe/mouthguard in your mouth
A tear in your oesophagus which normally heals by itself
Breathing problems. You may need medication to fix this
A large tear/perforation of your oesophagus. You may need surgery to fix this
An abnormal heartbeat that normally settles by itself
Death as a result of a TOE is extremely rare
Before Your Procedure
Do not eat anything 6 hours before your procedure, you may drink only clear fluids up until 2 hours before your procedure.
If you take Empagliflozin (Glyxambi®, Jardiamet®, Jardiance®) or Dapagliflozin (Forxiga®, Xigduo XR®, Qtern®) stop taking 3 days before.
Please let us know if you are allergic to any medications.
Ask any questions that you or your family may have before signing and consenting to the procedure.
Please arrange for a friend or family member to take you home from hospital and stay with you for your first night at home. You cannot go home alone or in a taxi or on public transport.
You will change into a hospital gown, an ID band applied.
The healthcare team will take your blood pressure and pulse and insert an IV (intravenous) line into a vein in your arm.
During the Procedure

If you have dentures or plates you will be asked to remove them before the probe is inserted.
The back of your throat will be sprayed with a local anaesthetic (numbing medication) to make passing of the probe more comfortable. You may experience a sour taste.
You will be asked to lie on a bed on your back or side and the room will be made dark.
A bite protector will be placed in your mouth.
You will be given some sedation medication through your IV to make you sleepy and relaxed. Oxygen will be given to you through small nasal tubes.
Once you are sleepy the probe will passed through your mouth and down your throat to your oesophagus (food pipe). You may be asked to swallow to help pass the probe.
Once the probe is in the right place ultrasound images are taken on the computer.
After all the images have been taken the probe will be removed and you will be moved to the recovery area for monitoring.
If no other tests or care is needed you may be able to go home 2-4 hours afterwards.
Activity After the Procedure & At Home
1 hour after your TOE you will be given a small amount of water to swallow. If you do not have any problems with swallowing you will be allowed to eat and drink after another hour.
Do not have any hot food or hot drinks on the day of your procedure.
Rest on the day of your procedure in a bed or recliner chair. Slowly return to normal activities the next day.
Restart your normal medication and insulin after your procedure.
Do not make any major decision or sign any important documents for 24 hours after your procedure.
Do not drink any alcohol or take medications that make you sleepy for 24 hours after your procedure.
Symptoms To Look Out For After Your Procedure
If you have any of the following please seek medical attention:
Back or chest pain
Shortness of breath
Continued difficulty swallowing
Blood in your bowel motions
Bleeding from your mouth or coughing up blood
Vomiting


Driving once you are home
Do not drive for at least 24 hours after your procedure.
More information can be obtained from your Cardiologist or the Roads and Maritime Services (RMS NSW).
Follow Up
Please see your local doctor in 3 days and make an appointment to see you Cardiologist in 4 weeks.
Cardioversion
Why Do I Need A Cardioversion?
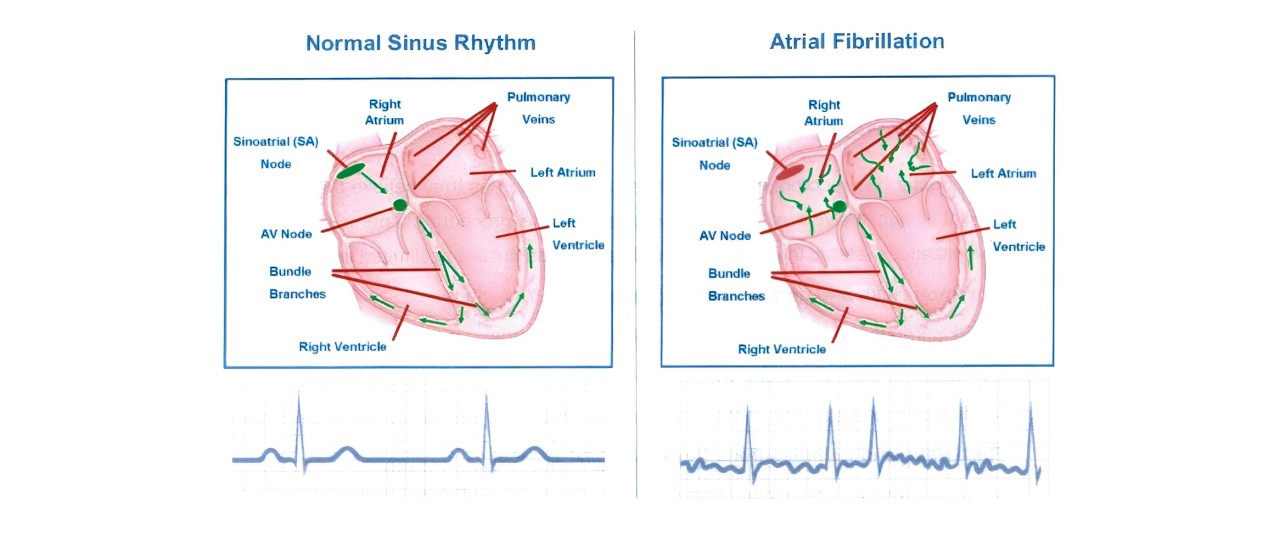
In Atrial Fibrillation (AF) or atrial flutter your top chambers (Atria) of your heart can beat irregularly and at times faster than normal. Sometimes your lower chambers (ventricles) of your heart can also beat very fast (ventricular tachycardia). This can at times make you to feel short of breath, have palpitations, get light headed or have blackouts.
A cardioversion is a procedure that is done to return your abnormal heart rhythm (such as atrial fibrillation or atrial flutter) to normal heart rhythm (sinus rhythm). An electrical shock is sent to your heart through gel electrode pads put on to your chest. You will be given medications to make you relaxed and sleepy (sedated) for the procedure. The procedure takes only a few minutes.

What are the risks?
Your doctor has recommended you for a cardioversion as they believe the benefits to you outweigh the risk of not going ahead with the procedure. There are risks and complications related to this procedure. They include but are not limited to the following.
Skin irritation or redness from the gel electrode pads.
Return of atrial fibrillation within 12-24 months.
The cardioversion may not be successful in returning you to normal sinus rhythm.
If you have an underlying heart condition you may need a pacemaker.
Stroke that may cause long term disability. To reduce this risk if you have been in atrial fibrillation for more than 2 days you will normally be on blood thinners such as warfarin for at least 3 weeks or have a transoesophageal echocardiogram (TOE) before the cardioversion to check for blood clots that might sit inside the heart chambers. Death as a result of a cardioversion is rare.
Before Your Procedure
Do not eat anything 6 hours before your procedure, you may drink only clear fluids up until 2 hours before your procedure.
If you take Empagliflozin (Glyxambi®, Jardiamet®, Jardiance®) or Dapagliflozin (Forxiga®, Xigduo XR®, Qtern®) stop taking 3 days before.
If you take Warfarin, Dabigatran (Pradaxa®), Rivaroxaban (Xarelto®) & Apixaban (Eliquis®) they need to be continued.
Please let us know if you are allergic to any medication.
Ask any questions that you or your family may have and sign a consent form.
Please arrange a friend or family member to take you home from hospital and stay with you for your first night at home. You cannot go home alone or in a taxi.
You will change into a hospital gown, an ID band applied
The healthcare team will take your blood pressure and pulse and insert an IV (intravenous) line into a vein in your arm.
Activity After The Procedure
If no other tests or care is needed you may be able to go home 2-4 hours afterwards.
Rest on the day of your procedure in a bed or recliner chair.
Restart your normal medication after your procedure.
Do not make any major decision or sign any important documents for 24 hours after your procedure.
Do not drink any alcohol or take medications that make you sleepy for 24 hours after your procedure.


Driving once you are home
Do not drive for at least 24 hours after your procedure.
More information can be obtained from your Cardiologist or the Roads and Maritime Services.
Follow Up
Please see your local doctor in 3 days and make an appointment to see you Cardiologist in 4 weeks.